What is Peripheral Arterial Disease (PAD)?
Peripheral arterial disease occurs when the arteries that pump blood from the heart to the extremities are narrowed or blocked. This is typically caused by a buildup of fatty deposits in the arteries (atherosclerosis) and most commonly affects the legs. Peripheral arterial disease can lead to debilitating pain, making it difficult for those affected to exercise or engage in daily activities and significantly impacting their quality of life.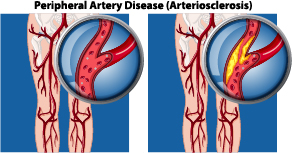
Symptoms of Peripheral Arterial Disease
The most common symptom of peripheral arterial disease is pain in the legs during exercise that goes away with rest. Other symptoms that appear in the affected leg include:
- Numbness, tingling, pain, cramping or weakness
- Coldness, especially when compared to the normal leg
- Hair loss
- Slowed toenail growth
- Shiny skin
- Changes to skin color
Risk Factors for Peripheral Arterial Disease
As with many vascular conditions, risk factors that increase the likelihood of developing peripheral arterial disease include high cholesterol, high blood pressure, smoking, diabetes, a family history of the condition, and being 60 or older.
Treatment for Peripheral Arterial Disease
In most cases, the first line of treatment is medication combined with lifestyle changes. Depending on the patient’s unique circumstances, medications to lower cholesterol or blood pressure, prevent blood clots, or reduce pain may be prescribed. Lifestyle modifications can include regular exercise, a low-fat diet, and quitting smoking.
More severe cases may benefit from minimally invasive interventional radiology procedures. During these procedures, a catheter is inserted into a small incision in the body and the physician relies on imaging guidance to thread it to the affected area. Once there, the physician may place a small balloon at the site of the block and inflate it to open the blood vessel (angioplasty); insert a small metal cylinder to hold the clogged vessel open (stent); or deliver clot-busting medication if the block is caused by a blood clot (thrombolytic therapy).
Traditional surgical procedures, such as bypass grafts, come with longer, more painful recovery periods. Because interventional radiology procedures use small incisions and imaging guidance instead of large incisions, the recovery times are much shorter and less painful. That means patients can get back to daily activities and enjoy an improved quality of life much sooner than with traditional procedures.
If you’d like to see if one of these minimally invasive solutions is the right choice for you, reach out to schedule an appointment with one of our doctors. Our expert interventional radiologists are here to help you feel better without the trouble of major surgery.